
Longreads
21 MIN READ

Incompetent political leadership and corrupt administration has meant no new doctors have been appointed in the past four years. This has caused a great deal of suffering for many Nepalis.

Before the second wave of Covid-19 started in Nepal, Tikapur Hospital in Kailali procured seven ventilators. But with few health workers and doctors available to operate the ventilators and provide critical care, many of those infected who came to the hospital lost their lives. As of May, 46 people died at the hospital due to the disease.
“We had the equipment, but couldn’t find the doctors to operate them. Many couldn’t be saved due to a lack of human resources to operate ventilators,” said Deepak Rawal, chairman of Tikapur Hospital.
The hospital has provisions for eight specialist doctors, including anaesthesiologists, and four medical officers (appointed by the government), but all the positions have remained vacant for years. Despite repeatedly issuing notices to appoint doctors on contract basis, the hospital has not received any application. "We appealed to the federal and the provincial governments, as we couldn’t find a doctor. But we got nothing but assurances,” said Rawal.
Tikapur Hospital is currently run by doctors hired on contracts with the help of donor organisations and those recruited under two-year scholarship programmes, various other schemes such as the safe motherhood programme, and campaigns run by local government. Medical Superintendent Rem Kumar Rai says, "Health care services can’t be run in a sustainable and reliable manner if they are run by doctors working under scholarship programs or those on contract."
The condition of Tikapur Hospital is a reality common to government and community hospitals across the country. The Auditor General's annual reports point out that a significant number of positions to be filled by doctors have remained vacant in government hospitals across the country for years.
The vacancies, which are to be filled by the Public Service Commission, have not been filled for the last four years because the Ministry of Health, the body that appoints doctors to state-run hospitals, has been reluctant to do so under the excuse that the adjustment of doctors at the federal and local levels after the country adopted federalism is yet to be completed.
Some hospitals have hired doctors at their own expense, but the burden of increased costs has been transferred to patients. A United Nations Children's Fund (UNICEF) and the European Union study on the cost of healthcare released in June states that the average Nepali family bears more than 50 percent of the cost of treatment from their own pocket. Former Director-General of the Department of Health Services Sushil Nath Pyakurel says, "This means that the people are not being treated with the money paid by taxpayers."
Reaching the hospital on time doesn’t save lives
As of September 30, 11,123 people have lost their lives due to Covid-19 across the country. A news report based on analysis of the Covid death data till mid June had found that 92 percent died in hospitals. Only five percent lost their lives at home, while less than one percent lost their lives on the way to the hospital and at isolation centers, according to the report published on the online news portal, Nepal Live, in collaboration with the Centre for Data Journalism (CDJN).
Among the many reasons behind the death of the infected who reach the hospital on time is the lack of adequate infrastructure and equipment, such as intensive care units and ventilators. Lack of specialist doctors is another major problem faced by hospitals. Dr. Subash Acharya, in-charge of the intensive care unit at TU Teaching Hospital, says, “The number of ICUs and ventilators is negligible compared to the population we serve, and the human resources available is even less.”
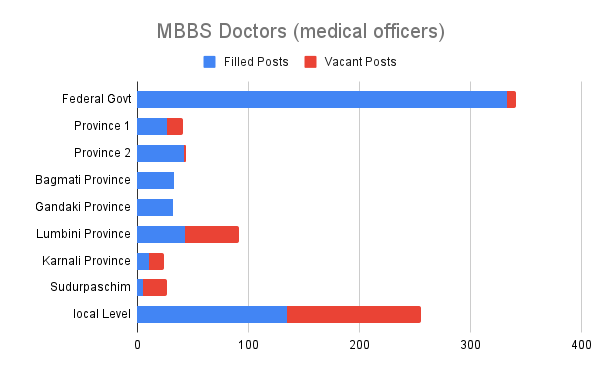
According to the Ministry of Health, 70 percent of the 793 positions created for specialist doctors at government hospitals across the country are currently vacant. Although 890 posts have been allocated for doctors with a graduation degree in medical education (MBBS), 25 percent of the posts are vacant. A total of 15 percent of those MBBS doctors on the job are on study leave.
It is clear from the figures that at a time when the number of positions allocated is already low, only half of the doctors are providing services. The Auditor General's Annual Reports also mentions that patients admitted to government hospitals need to be referred elsewhere due to the non-filling of vacancies in approved posts, and this has affected the delivery of services.
Mass exodus amid shortage of doctors
Even during this shortage of doctors, it has been four years since the Public Service Commission issued vacancy calls to fill existing posts. Ever since a vacancy for 100 doctors was announced in 2017, not a single permanent doctor has been inducted into government service.
Even doctors who have received scholarships to complete their medical education have gone abroad, as the hiring process of the health workers are halted. Doctors who enter government service receive the opportunity to complete their MD/MS degrees through government scholarships, and for this reason, many doctors aspire to work for government hospitals. But with the Public Service Commission not conducting exams, they too have decided to go abroad.
A report by the Centre for Investigative Journalism, Nepal, published in January 2020, revealed that more than 50 percent of doctors who studied on government scholarships have gone abroad. The number of doctors going abroad had been high following the Public Service Commission’s reluctance to conduct exams, the trend has intensified further amid the Covid-19 pandemic. "The number of specialist doctors going abroad has increased recently due to the lack of the option to join the public service," said Dr. Kirtipal Subedi, general secretary at the Government Doctors’ Association of Nepal (GODAN).
Countries including the United States, Canada, and the United Kingdom offer attractive packages, including the opportunity to complete higher education, to doctors who have studied on government scholarships. It is estimated that in the last four years, about 400 doctors have gone to the United States alone to pursue their MD degrees. The number of doctors going to Canada and the United Kingdom is also significant.
Kedar Bhakta Mathema, chairman of the High-Level Task Force on National Medical Education Policy 2015, says, if doctors who studied on scholarship continue to go abroad the way they are now, the government's investment in education is a waste of money. “The reason the doctors get a scholarship is that they are to stay in the country to serve the people,” he said.
Along with the delay in filling government posts, the low salary on offer is also another reason doctors are going abroad. The salary paid by a private hospital to a new doctor is usually Rs 30,000 to 40,000, which pales in comparison to what a doctor can make abroad.
The maze called ‘adjustment’
Since the country adopted federalism, around 26,000 health workers, including 242 specialist doctors and 665 medical officers at the federal, provincial, and local levels have been adjusted. Among them, 82 percent (22,103) health workers serve at the local level, 8.6 percent (2,308 people) at the provincial level, and 8 percent (2,151 people) at the federal level.
However, the Ministry of Health has remained silent on the recruitment of doctors, saying that it still needs to manage the grievances of serving doctors.
Ministry spokesperson Dr. Krishna Prasad Poudel admits that the recruitment of doctors hasn’t resumed since the adjustment process began. “Positions have remained vacant and this has affected health services,” he said.
When asked about the reason for the suspension of recruitment, the then Joint Secretary of the Administration Division Damodar Regmi said that he had not requested the Public Service Commission to recruit new doctors as he had yet to address grievances presented by serving doctors about their adjustment. “But we will announce vacancies for around 150 doctors by mid-September after around 5 percent of the doctors working at the federal level retire from service,” he added.
However, there are more health workers at the provincial and local levels compared to that at the federal level. And not all the provincial public service commissions are ready to recruit doctors. Even during the first wave of the Covid-19 pandemic, the federal government couldn’t send doctors to the worst-hit areas as people died in remote parts of the country. And the main reason this happened was that the recruitment of health workers remained halted.
Some local and provincial governments that faced difficulties treating Covid-19 patients had also appealed to the provincial public service commissions to recruit doctors. The public service commission in Lumbini Province in September 2020 and the Bagmati Province in November issued vacancies for various posts. However, the federal government, which has shown no interest in hiring health workers, wrote to the commissions not to go ahead with the recruitment, as the adjustment of staffers had not been completed. Health Secretary Laxman Aryal wrote to all the provincial public service commissions in November 2020 to halt the recruitment of doctors. Baburam Gautam, a member of the Lumbini Public Service Commission, said: “During the Covid-19 pandemic, the health ministry neither sent doctors to the provinces nor allowed them to recruit doctors on their own.”
However, the Lumbini and Bagmati Public Service Commissions ignored the ministry's letter. The final results of exams conducted for nurses, health assistants, and lab technicians are yet to be published in Bagmati. Chairman of the commission Sureshman Shrestha says that vacancies for 26 posts, including that for nine medical officers, will be issued with priority. Meanwhile, the vacancy call issued by the Lumbini Provincial Public Service Commission last September for 49 medical officers, seven nursing officers, five physiotherapists, and five medical lab officers has been on hold following a writ petition filed at the Supreme Court.
The Public Service Commission of Province-2 has issued a call in the last week of June, but it will still take months to appoint new doctors. Gautam, a member of the Lumbini Provincial Public Service Commission, said, “Many local and provincial hospitals tried to appoint doctors on contract during the pandemic, but no applications were received. If we had issued a call for permanent appointment, things would have been different, but the federal government hasn’t done so.”
While no new doctors have been hired in the last four years, four secretaries have assumed office at the Ministry of Health: Dr. Pushpa Chaudhary, Ram Prasad Thapaliya, Yadav Prasad Koirala, and Laxman Aryal. Dr. Roshan Pokharel is currently secretary.
Meanwhile, Bhanubhakta Dhakal, Hridayesh Tripathi, Sher Bahadur Tamang, and Krishna Gopal Shrestha have taken charge as Minister for Health at different times during the course of the pandemic. Umesh Shrestha is now the Minister of State for Health. However, no one has tried to fill the vacant positions for doctors.
When inquired about why the recruitment of human resources had been stopped for four years, Dr. Gunaraj Lohani, chief of the Policy, Planning and Monitoring Division at the ministry, said, "The exams for the appointment of health workers has been halted as there is a vacancy in the Public Service Commission itself."
Despite Lohani's claim, the Ministry of Health has not sought the appointment of doctors. On top of that, positions at the commission became vacant only a short time ago. Devi Prasad Subedi, information officer of the commission, said, "The Ministry of Health hasn’t asked us to recruit doctors in the last five years."
General Secretary of Government Doctors Association of Nepal (GODAN) Dr. Kirtipal Subedi said the problem surfaced after the management of the health workers were delegated to three levels of government.
“The Health Service Act 1991 classified health services as technical services. Now, after the adjustment, the chain of command from the bottom to the top has been broken. That is why the federal government has been unable to send doctors to the area where the epidemic spread,” said Dr. Sushil Nath Pyakurel, former director-general at the Department of Health Services, adding that the government decision to merge the health service with the general civil service reminds him of the Panchayat period.
The negative role played by the federal government in the recruitment and management of human resources in health services is not limited to this. The Federal Civil Service Bill, considered important for the professional development of all government employees, has been stuck in Parliament for two and a half years. Due to the stalemate, the provinces have been unable to enact laws related to career development of health workers. In the absence of provincial laws, it is unclear how doctors appointed at the local level will fare in the future.
60 percent posts vacant in Province 2
The worst is taking place in Province-2, which lags in all aspects of education and health in the Human Development Index. In every review meeting held at the office of the Chief Minister or the ministries, it is reported that about 60 percent of health worker’s posts in the province are vacant.
An example of how poor the province’s healthcare is can be seen at the district hospital in Malangawa, Sarlahi. The hospital has a ventilator, but it doesn’t have a specialist doctor to operate it. The contract to purchase equipment worth Rs 30 million to build infrastructure for the neonatal intensive care unit (NICU) is in the final stage, but no pediatrician is being sought.
The posts of all the eight specialist doctors and three of five medical officers at the hospital have been vacant for years. Five fresh MBBS doctors recruited under a provision of mandatory two year services for scholarships are running the hospital.
Nawal Kishor Jha, who became medical superintendent of Malangwa Hospital in April after heading the health division at the Ministry of Social Development of Province-2, said, “We have asked the Public Service Commission to recruit doctors, but it hasn’t issued any vacancy announcements.”
The story of Siraha, Gaur and Janakpur hospitals is no different than that of Sarlahi. Acting Medical Superintendent of Siraha Hospital Dr. Nagendra Yadav is the only specialist doctor of the hospital, which has provision for 10 specialist doctors. Admitting that the hospital, which was upgraded from 15 to 50 beds five years ago, hasn’t written to the Public Service Commission (the provincial commission after 2018) Dr. Yadav said, “The commission had verbally asked us about the doctors, but didn’t seek anything in writing.”
Nineteen of the 25 specialist doctors’ positions at Janakpur Hospital are vacant. The Province-2 Public Service Commission issued vacancy calls for seven specialist doctors in May. Then, in July, it issued calls for 17 specialist doctors and two medical officers. According to Spokesperson Gangesh Gunjan Jha, the commission is yet to announce vacancies for other health workers including nurses.
Hospitals should send their requirements for health workers to the Public Service Commission through the Ministry of Social Affairs, which forwards the request to the Chief Minister's Office. The CM’s Office then communicates with the Public Service Commission. So the hospitals themselves do not seek to hire doctors or if they do, their requests get stuck at the Ministry of Social Development or the Chief Minister's Office. Efforts to know how many healthcare-related recruitment requests have been sent to the federal and provincial public service commissions in the last four year were in vain. Multiple efforts to get answers from Yam Prasad Bhusal, spokesperson for the Chief Minister's Office; Bishnuraj Dhakal, Bhusal’s superior; and Chief Secretary Gokarnamani Duwadi did not turn out to be fruitful.
The Health Service Act states that officials concerned must inform the Public Service Commission within a month after a position falling vacant. The law says officials who don’t report vacancies within the period are liable to face departmental action. So far, however, no such action has been taken.
Nepotism in hiring doctors on contract
Our research showed that government hospitals are primarily staffed by doctors on scholarships. Janakpur, Siraha, and Malangwa hospitals are representative examples of this. As those who became doctors on government scholarships need to serve at public hospitals for two years, the tendency of hospitals not to recruit permanent doctors has taken root. They appoint three or four doctors on contract at a time and then hire another group when their term ends so that there is no need to hire permanent doctors.
The federal government's reluctance to fill the vacant positions has also created an opportunity for some hospital administration leaders to appoint temporary doctors instead of recruiting permanent doctors. A doctor at a government hospital said without any qualm that as the federal government pays temporary doctors the same salary it would pay permanent doctors, hospital administrators are hiring their relatives for the job.
A specialist doctor at Lumbini Provincial Hospital, Butwal, who didn’t want to be named, said: “One of the reasons why the recruitment process has been stalled is that hospital administrators these days get to hire doctors related to them.” He added that it was not a coincidence that these days the hospital administration is more interested in appointing doctors on contract and the staff adjustment is taking time to resolve.
Another specialist doctor working at the Hetauda-based provincial hospital who wants to remain anonymous said that vacancies are even kept secret and they never make it to the Public Service Commission. Choosing to remain anonymous, he said, "The reason for this is that some doctors working at the hospital don’t want to share the money they make by working in private clinics in the morning and evening. In cahoots with the hospital administration, they won’t allow officials to demand new doctors through the public service commission.”
In the midst of the Covid-19 epidemic, on May 28, 2020 the then Finance Minister Yubaraj Khatiwada announced the policy of 'one doctor / health worker, one institution' in his budget speech. After seven months, on January 4, the Council of Ministers also passed the working procedure in this regard. The preamble of the procedure states that "a working environment will be created by discouraging the practice of doctors and health workers working in more than one health facility." Similarly, the health workers can get up to 100 percent of their salary as an allowance.
However, the Ministry of Health has not made the procedure public till date. General Secretary of GODAN Dr. Kirtipal Subedi says, "Even if the government implements this policy by providing attractive facilities, it seems that it is only trying to push it without considering other aspects of the decision."
Former Director-General at the Department of Health Services, Dr. Sushil Nath Pyakurel, says, “The procedure seeks to streamline overall healthcare rather than directly encourage doctors. Their service will be efficient only if the government provides the required human resources and infrastructure to the hospital.”
Apart from newly opened primary health centers and special hospitals, the number of doctor positions in the country’s public healthcare system hasn't increased since the early 1990s when the country’s population was just 20 million. According to Dr. Pyakurel, one of the reasons the ministry doesn’t understand the plight of the 26,000-strong public healthcare sector is that a doctor hasn’t been appointed secretary at the Ministry of Health in recent years.
A survey was conducted on the number of manpower required in the health sector of the country to adjust the health workers in federal set-up, but no new posts were added. The existing manpower was shuffled around. The Economic Survey for the fiscal year 2019/20 shows that 2,640 doctors are working in government hospitals across the country. The World Health Organization (WHO) says that by 2030, 6.64 doctors per 10,000 population will be needed to achieve the Sustainable Development Goals. Similarly, the body also says there should be 23 nurses and midwives and 14.83 other health workers. Overall, 44.5 health workers are needed for every 10,000 people.
But at present, the number of permanent nurses working in government hospitals is only 1,692. Similarly, the number of auxiliary nurse midwives (ANM) stands at 8,263. According to the Economic Survey 2019/20 there are 20,653 nurses and ANMs working in public hospitals around the country. About half of them (around 10,000 nurses and ANMs) are working on contract.
Government's priority: 'populist' programmes and buildings
In the 15 months since the outbreak of the Covid-19 pandemic, health workers have found themselves in dire straits. Even in such a situation, the appointment of health workers was not prioritised by the government. The federal budget for the previous fiscal year, which coincided with the pandemic, and this year's budget for the second wave of the disease do not even mention the appointment of permanent doctors.
Similarly, no plan or package has been brought to send doctors living in urban areas to the remote ones. So much so that last year, doctors and health workers on the frontline were frustrated by the untimely payment of 100 percent of their basic pay. Later, authorities said that risk allowance would be given only to those doctors working between April to July 2020. However, the allowance was not paid on time. Dr. Ajit Mallik had to sit-in for 28 days just to receive the incentive allowance for working for four months in the treatment of Covid-19 patients at the TU Teaching Hospital, Maharajgunj.
During the second wave of infections, the risk allowance for doctors and health workers involved in the treatment by taking more risks was slashed. In his address to the nation on May 3, four days after a lockdown was announced due to the second wave, the then Prime Minister KP Sharma Oli had reduced the 100 per cent incentive allowance to 50 per cent from the previous year.
The then Finance Minister Bishnu Prasad Poudel increased the old age allowance by Rs 1,000. While most of the senior citizens were losing their lives due to Covid-19 and lack of treatment, the government has allocated Rs 16.90 billion on old age allowance for the current fiscal year. However, just one-third of the expenditure (Rs 5.63 billion) could have been used to pay double the number of existing specialist doctors and physicians, but also an additional 10,000 nurses.
Economist Keshav Acharya says, "The government could have created new postings for doctors instead of deciding to increase its recurring financial burden, but it got stuck with cheap popularity."
Four years ago, the Pushpa Kamal Dahal-led government launched the Health Infrastructure Standards and Integrated Health Infrastructure Development Project. Officials had spelled out the number of health institutions to be built under the three tiers of government by 2024 and the human resources needed to run the facilities.
The plan was to build 3,329 health posts, 733 primary hospitals, 15 second-tier hospitals, 15 tertiary hospitals, eight central specialty hospitals, and eight teaching hospitals during the period.
Similarly, the number of medical officers would be increased from 1,367 to 6,300, the number of specialist doctors from 671 to 3,300, and the number of nurses to 30,000.
According to the same plan, the then Prime Minister KP Sharma Oli laid the foundation stone of 396 hospitals (5 to 15 beds) in each local level on December 20, 2020. Prime Minister Oli, who was eager to spend nearly Rs 58 billion on the buildings, was not sensitive about recruiting the necessary health workers to run these facilities. Gagan Thapa, the then health minister of the Dahal-led government who led the formulation of both the plans, said, “The government cherry-picked the plan to build hospitals and procure equipment. But for some unknown reason, it didn’t launch any program to recruit health workers who would attend to the sick.”
Dr. Pyakurel, chief health specialist at the Ministry of Health, says, “Two to three doctors are essential in all of the 753 local level hospitals. In that sense, at least 1,500 to 2,000 new doctors are needed. However, the government hasn’t given the recruitment of health workers a thought.”
The first and the second wave of Covid-19 serve a lesson that equipment, including ventilators, can be procured, but essential human resources can’t be mobilized on short notice. Former Health Minister Thapa says, "We have repeatedly urged the leaders through Parliament to make plans and programs for healthcare professionals, but no one understands or doesn’t want to understand the situation."
According to economist Keshav Acharya, the collusion between the government's leadership, high-level administrators, and contractors and suppliers are the reason authorities focussed on equipment and buildings rather than doctors and nurses. Former member of the Nepal Medical Council Dr. Sushil Koirala, on the other hand, alleges that the construction of the hospital building was prioritised as the appointment of doctors doesn’t entail any additional benefits. He says, “If we want to appoint as many doctors and nurses as we need right now, we have to manage the human resources efficiently and also provide the necessary equipment. Health officials are not aware of this.”
Dr. Arun Upreti, who studied on a government scholarship, is doing his postgraduate studies at the Teaching Hospital in Maharajgunj after completing two years of compulsory service at the Charikot District Hospital in Dolakha. In his experience, “It is so difficult to work in a village without the necessary equipment and human resources, that only despair prevails.”
Former Vice-Chancellor of Tribhuvan University Kedar Bhakta Mathema says that a good salary and allowance are not enough to send the doctors to the village and keep them there, but also to stay there. "There should be good schools for the children of those doctors, otherwise they will not stay in the village," says Mathema.
However, the government has brought a 'one doctor/health worker, one health institution policy' to keep doctors in the village. However, because it is not practical, it can’t be implemented. Paediatrician Dr. Satish Koirala says that it is not possible if doctors are paid a wage that’s not even enough to sustain.
Former Minister of Health Gagan Thapa says, “Stopping an MD or PG doctor from working in another hospital without increasing government services is a very illegitimate step. That doesn't solve the problem.”
The government was expected to provide equipment and manpower to the remote areas during the pandemic. But all eyes were on the interests of private medical colleges and private hospitals. That Dr. Krishna Giri, vice-chairman of the Medical Education Commission, was coerced by the Oli government to provide affiliation to a sub-standard B&C Hospital as a medical college is a strong example of this. Dr Arun Upreti says, "PM Oli's move is enough to understand that the government prioritises profit-making medical colleges over the appointment of permanent doctors."
This article was previously published in Nepali by the Centre for Investigative Journalism, Nepal.
Rudra Pangeni Rudra Pangeni is an investigative journalist affiliated with the Centre for Investigative Journalism, Nepal. He is a 2019 Bertha Fellow.


Explainers
16 min read
The Oli government’s corrupt involvements in the procurement deals for lifesaving PPEs and test kits
COVID19
News
3 min read
Preventing coronavirus spread in Nepal’s overcrowded jails is becoming near impossible
Features
7 min read
The government’s failed Covid response is another indication of its unwillingness to uphold its constitutional responsibility
Features
3 min read
New ordinances signed by the President aimed at reducing acid attacks which have been on the rise in Nepal in recent years
COVID19
News
3 min read
A daily summary of Covid19-related developments that matter
Features
COVID19
5 min read
The strict protocols around the PM’s safety contradict the government’s overall lacklustre Covid response
Features
5 min read
As no formal orders have been placed and no agreements drawn up, even the Health Minister is looking to the gods.
Features
6 min read
New ICE regulations could force international students to return home